Evaluating ergonomics in healthcare – paramedics
The chance that a paramedic suffers an injury is 3x higher than other occupations. Because of the global health worker shortage, we need to make sure these professionals are taken care of.
Posted by
Published on
Wed 12 Feb. 2020
Topics
| Communication | Healthcare | Human Factors | Medical Simulation | The Observer XT |
The chance that a paramedic suffers an injury is 3x higher than other occupations. The cause of 94% of these injuries is a musculoskeletal disorder (MSD) like back pain, strains, and sprains. Because of the global health worker shortage, we need to make sure these professionals are taken care of.
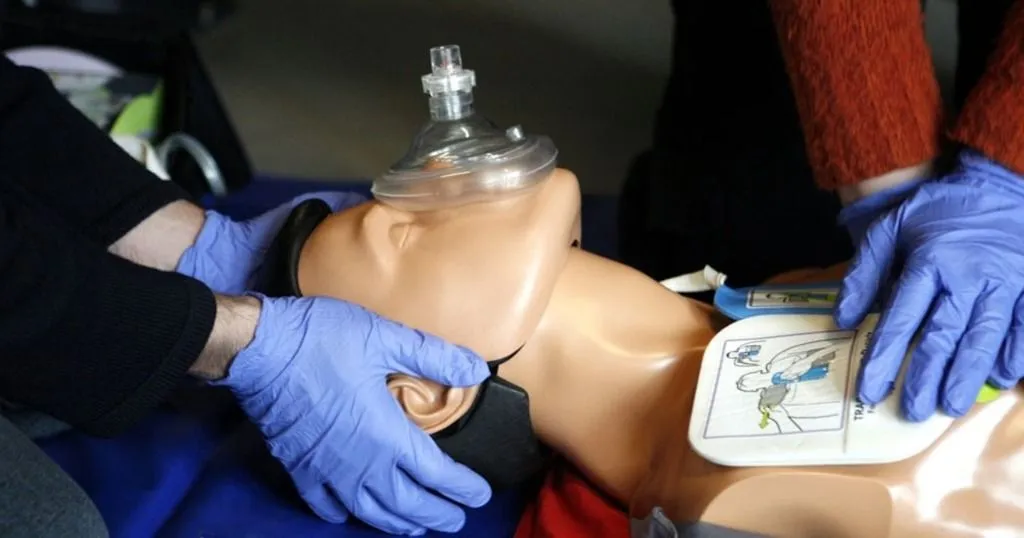
That’s one of the reasons Yaar Harari and colleagues from Ben-Gurion University of the Negev, Israel, and Magen-David-Adom (Israeli National Emergency Medical Services) decided to focus their research on improving human behavior in healthcare – specifically paramedic behaviors in relation to the equipment they have to use for both in- and out-of-hospital cardiopulmonary resuscitation (CPR).
Harari and colleagues evaluated out-of-hospital CPR because this situation is very demanding for these professional and there are no clear guidelines on how to use their equipment in these kind of situations. Improving the details in such a workflow and providing clear guidelines might make a huge impact on the injury rate and improve healthcare in general.
Observing simulations of a cardiac-arrest scenario
Twelve paramedic teams participated in two 10-minute in-situ simulations of a cardiac-arrest scenario. The researchers invited all the teams to the Human-Systems Integration in Healthcare Lab at the Ben-Gurion University of the Negev, Israel.
In order to capture all the behaviors in detail, all simulations were video-recorded from four angles using MediaRecorder software. The Observer XT professional research software allowed the scientists to observe the paramedics’ interactions with the equipment around the patient. You can see an event as an interaction in which the bag was either moved or used without being moved.
The researchers explained that they used a marked grid on the ceramic tiled floor (which is very common in homes and buildings in Israel) to help them define the position of each bag at the precise moment the interaction began and ended.
The researchers measured work efficiency by calculating the time each person spent on CPR as compared to other activities. CPR quality was measured by taking standard resuscitation measures and evaluating them (compression depth, rate, etc.).
Measure posture and push/pull of the bag
In the scenario the researchers also paid attention to how much strength it took to push and pull the bag via the physiological signals of the paramedical professional, such as heart rate and level of exertion. Both measurements may predict the level of fatigue of the professional.
Biomechanical load was assessed using direct measurements (number of times the equipment bags were handled and the cumulative force during the simulation that was required to move the bags) and ergonomic assessments (risk level for MSD based on the paramedics’ postures and loads, the range of spinal compression forces acting on the paramedics when they lifted, pushed, and pulled the bags).
Results
The study results show that the initial positions of the equipment bags influence clinical measurements of CPR quality, as well as measures of the paramedics’ work efficiency, effort, and biomechanical loads.
Improving CPR quality and patient outcomes, and reduce paramedics’ risk of injury
Yaar Harari and colleagues demonstrated with these simulations that 72% of paramedics’ postures were categorized as high or very high risk for musculoskeletal disorders. This calls for action!
The researchers call for a discussion about the positioning and handling of the equipment bags during out-of-hospital CPR when seeking to improve paramedics’ performance and reduce their risk of MSD.
These guidelines related to bag positioning and equipment handling might also improve CPR quality and patient outcomes, as they found that paramedics wasted time moving around the patient in order to reach their equipment.
Reference
- Harari, Y.; Riemer, R.; Jaffe, E.; Wacht, O.; Bitan, Y. (2020). Paramedical equipment bags: How their position during out-of-hospital cardiopulmonary resuscitation (CPR) affect paramedic ergonomics and performance. Applied Ergonomics, 82.
- https://www.weforum.org/agenda/2019/07/5-ways-to-bridge-the-global-health-worker-shortage/
Related Posts

Learn to cooperate toward shared goals using the principles of CRM

Observations of surgeons as a tool to assess competency

